
Anatomy
The Portal Vein is made up three main vessels the Superior and Inferior Mesenteric veins and the Splenic vein. When these three vessels converge they become the Main Portal Vein which enters the Liver via the porta hepatis along with the hepatic artery and common bile duct (cbd exits the liver), aka the Portal Triad.

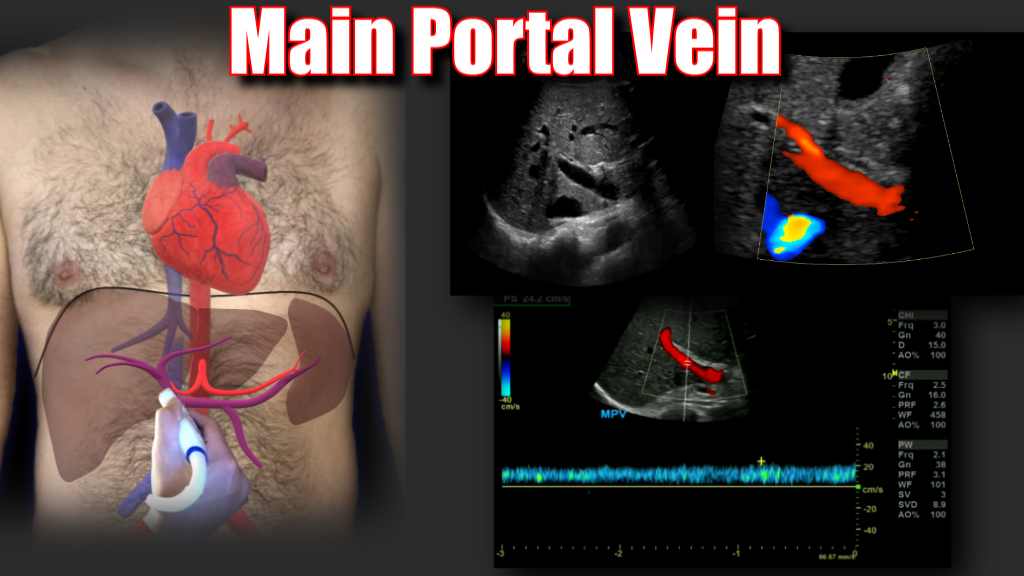
Main Portal Vein and Bifurcation
When the portal vein enters the liver it bifurcates into right and left main branches. The right portal vein bifurcates into an anterior and posterior branch which feed segments 5, 6, 7 and 8 respectively, whereas the left branch feeds segments 2, 3 and 4. The normal diameter of the main portal vein is 1.3 cm (some institutions use 15. as the upper limit) Normal flow is hepatopetal (towards the liver), with a flow velocity between 15-40 cm/s. Be sure to make sure you color is inverted and your approach is optimized. In the main portal vein below flow is hepatopetal in both images, the only difference is transducer angle, tilt and approach.

Portal Vein Bifurcation


Protocol
Portal Vein Thrombosis
Approximately 25% of cirrhotic patients can develop portal vein thrombosis, Oftentimes due to portal hypertension and sluggish flow through the fibrotic liver. Stagnant blood flow is more prone to coagulation. Any hypercoagulable condition can lead to portal vein thrombosis. (i.e. cancer, pregnancy, coagulopathies, COVID 19 to name a few).
Common causes differ by age group:
- Newborns: Infection of the umbilical cord stump (at the navel)
- Older children: Appendicitis (infection can spread to the portal vein and trigger the formation of blood clots)
- Adults: polycythemia, certain cancers (liver, pancreas, kidney, or adrenal gland), cirrhosis, injury, disorders that make blood more likely to clot, surgery, and pregnancy.
Symptoms
Many people diagnosed with PVT are asymptomatic, some patients may have ascites, abdominal pain, hepatosplenomegaly, blood in the stool, bloody emesis (from ruptured varices). When the thrombus causes portal hypertension or if there is portal hypertension form cirrhosis, portosystemic collaterals may form. These sites of include:
- Esophageal varices
- Gastric varices
- Recanalized paraumbilical vein
- Splenic varices and splenorenal shunt
- Rectal varices and hemorrhoids
Often, several conditions work together to cause the blockage. The cause is unknown in about one third of people.





Transjugular Intrahepatic Portosystemic Shunt (TIPS)
A TIPS procedure may be used to reduce portal hypertension and its complications, like variceal bleeding. Usually done by an interventional radiologist, a small wire-mesh coil (stent) into portal vein. The stent forms a shunt that bypasses the liver. This channel reduces pressure in the portal vein. By reducing portal hypertension, varices are less likely to rupture and bleed. And other complications of cirrhosis like ascites may improve.

























Excellent
LikeLike